Challenges in breast cancer diagnostics
In 2022, breast cancer was the second-most common cancer type in the total number of cancer incidents, right after lung cancer.1 Over the next 20 years (2025-2045), WHO’s International Agency for Research estimates that the number of new breast cancer cases will increase from 2.45 million to 3.36 million worldwide.2 This has and will continue to place a significant burden on pathologists, an already underrepresented group of healthcare professionals. Meanwhile, the traditional tools used by pathologists do not keep pace with the increasing demand in their field.
Pathologists devote a significant amount of their time to analyzing tissue slides, a task that is highly detailed and manual in nature. Because this work is laborious, and labs face rising case volumes along with a shortage of pathologists, patients may experience delays in receiving diagnosis and treatment decisions. Reliable, efficient clinical tools can support pathologists and help patients receive timely, consistent care.
Current methods for breast cancer grading and biomarker scoring are particularly prone to variability. For example, commonly used scoring schemes require pathologists to extract quantitative parameters that are subject to inter- and intraobserver variability. The need for objective and standardized tools is evident. This lack of standardization has driven the search for an objective, automated technology.
To address this need for standardized tools, deep learning artificial intelligence (AI) has been utilized to automate and streamline repetitive quantification tasks in the pathology workflows. AI analyses can be consistently replicated across different tissue processing parameters and varying levels of complexity in region-of-interest (ROI). This capability makes AI analysis robust against biases and fatigue, which often hinder traditional analysis methods. As a result, AI becomes an invaluable asset in pathology workflows, delivering high-throughput, objective, and reproducible output that supports pathologists in the diagnostic interpretation.
AI-assisted data and decision support
AI can help pathologists and patients overcome the issues of diagnostic delays and variability. By automating time-consuming manual tasks, AI can count cells and biomarkers, or identify tissue areas in a fraction of the time that humans can, allowing pathologists to deliver timely and accurate diagnostics.
According to a systematic review by Jeong J et al., AI applications can cut medical diagnosis time by over 90%, significantly improving workflow efficiency and lowering the workload for medical professionals.3 Based on Aiforia’s clinical validation study, integrating AI into breast cancer image analysis workflow shortens the average analysis time per slide by up to 54%. This substantial time saving per slide enables pathologists to dedicate more time to complex cases and helps laboratories to reduce diagnostic backlogs and to facilitate faster treatment decisions for patients.
In addition to its clinical benefits, AI can help reduce costs and balance workload distribution. Reducing diagnostic error and misdiagnosis while improving treatment accuracy with more detailed results will provide direct cost savings due to greater precision. With fewer manual, repetitive, and time-consuming tasks, pathologists can focus their time and energy on rare or complex cases that require more in-depth analysis expertise.
Read more about the benefits of using AI in clinical diagnostics: 5 reasons to use AI in clinical diagnostics
Breast cancer diagnostics tools: Aiforia’s CE-IVD marked AI solutions
Aiforia® Breast Cancer Suite provides a fully integrated digital cockpit for breast cancer diagnostics, tailored to support the entire diagnostic workflow. This comprehensive solution includes an extensive set of CE-IVD marked clinical AI models for breast cancer, accessed through an intuitive and interactive user interface, Aiforia® Clinical Suite Viewer.
The core of this Clinical Suite is defined by a powerful AI model portfolio designed for automated histological grading from H&E-stained digital slide scans and the objective quantification of the key breast cancer IHC biomarkers to support pathologists:
- Aiforia® Breast Cancer Grading automates breast cancer grading from H&E-stained whole-slide images (WSI), accurately identifying invasive carcinoma and ductal carcinoma in situ (DCIS). It objectively scores mitotic count, tubular formation, and nuclear pleomorphism, addressing key challenges of manual grading such as variability and time constraints, consistent with the Nottingham Grading System.
- Aiforia® Breast Cancer ER automatically detects invasive carcinoma and quantifies ER-positive and negative tumor cells from whole-slide images (WSI) or selected tissue areas, supporting consistent and objective scoring.
- Aiforia® Breast Cancer PR automatically detects invasive carcinoma and quantifies PR-positive and negative cells from whole-slide images (WSI) or selected tissue regions, enhancing diagnostic clarity and workflow.
- Aiforia® Breast Cancer HER2 accurately identifies invasive carcinoma and scores HER2 expression in alignment with CAP guidelines, improving diagnostic reliability and workflow efficiency.
- Aiforia® Breast Cancer Ki67 automatically detects invasive carcinoma and quantifies Ki67-positive and negative tumor cells from whole-slide images (WSI) or targeted image regions, improving diagnostic accuracy and workflow.
- Aiforia® Lymph Node Metastasis automatically detects and quantifies metastases from breast cancer in whole slide images (WSI) of lymph node biopsies.
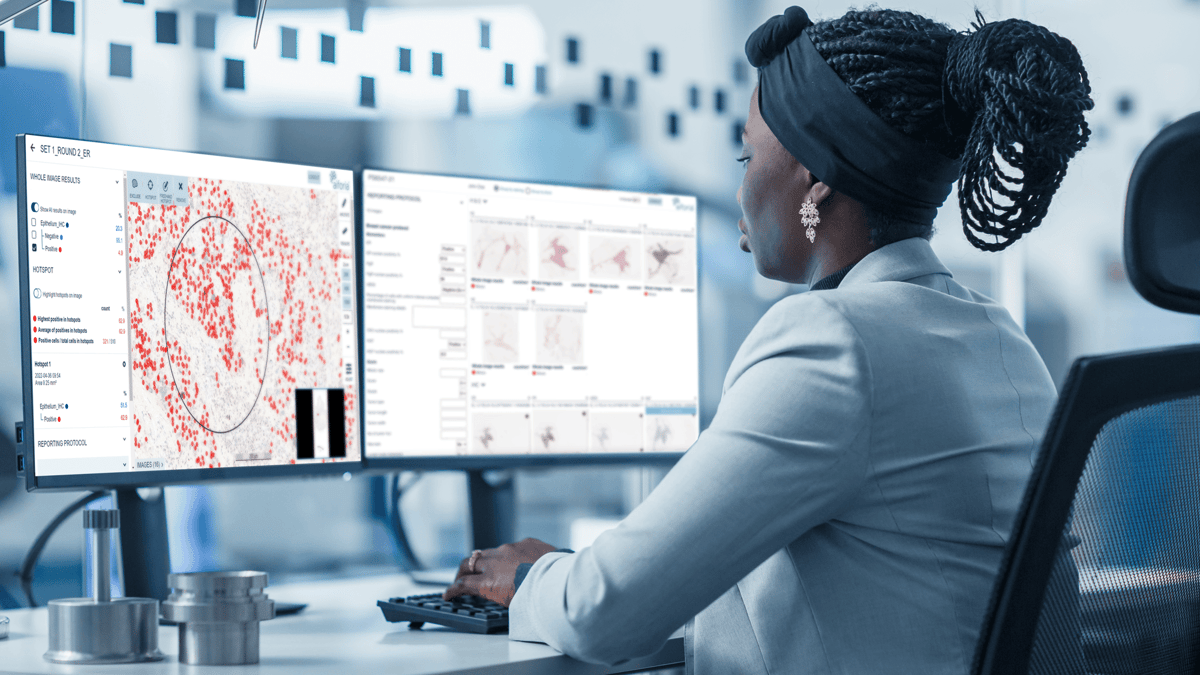
The CE-IVD marked Aiforia® Clinical Suite Viewer enables the rapid display and interactive review of analysis results generated by Aiforia's deep learning AI models. The Clinical Viewer offers an intuitive and easy-to-understand user experience. Furthermore, it allows pathologists to review, verify, and modify AI model output on top of the original slide scan image, providing essential human oversight to maximize the quality of final results. The AI results and scores are directly populated into a reporting panel, both at the slide and case levels. The results navigator helps to find rare objects in order of confidence, a certainty score that the AI model assigns to each detected object. Seamless integration into existing laboratory systems enables the results to be automatically transferred to LIS/LIMS and trigger subsequent testing workflows, such as IHC ordering upon detection of invasive carcinoma (BC Grading).
Further reading:
- Harmony on the horizon – could AI standardize breast cancer grading?
- How can AI assist in detecting HER2-low breast cancer?
- Memorial Pathology case study: implementing AI in a private hospital setting
References
1. Global Cancer Observatory. (2025, November 28). Cancer today: Absolute numbers, Incidence, Both sexes, in 2022. https://gco.iarc.fr/today/en/dataviz/pie?mode=cancer&group_populations=1
2. Global Cancer Observatory. (2025, November 28). Cancer tomorrow: Estimated number of new cases from 2025 to 2045, Both sexes, age [0-85+]. https://gco.iarc.fr/tomorrow/en/dataviz/isotype?cancers=20&single_unit=100000&sexes=0&years=2045
3. Jeong J, Kim S, Pan L, Hwang D, Kim D, Choi J, Kwon Y, Yi P, Jeong J, Yoo SJ. Reducing the workload of medical diagnosis through artificial intelligence: A narrative review. Medicine (Baltimore). 2025 Feb 7;104(6):e41470. doi: 10.1097/MD.0000000000041470. PMID: 39928829; PMCID: PMC11813001.